Nclex questions acute kidney injury – NClex questions on acute kidney injury (AKI) challenge nurses to demonstrate a comprehensive understanding of this critical condition. AKI can arise from various etiologies, manifesting with distinct clinical presentations and necessitating prompt diagnosis and management. This article delves into the intricacies of AKI, equipping nurses with the knowledge and skills to provide optimal care for affected patients.
Etiology and Risk Factors
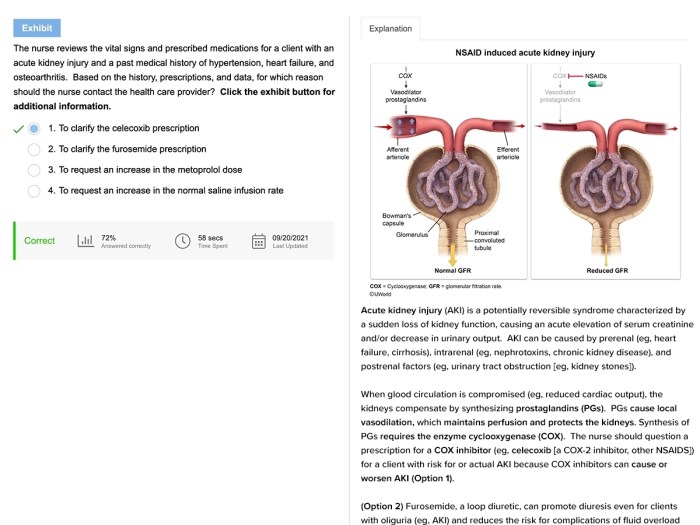
Acute kidney injury (AKI) can be caused by a wide range of factors, including:
- Prerenal causes: Conditions that reduce blood flow to the kidneys, such as hypovolemia, hypotension, and shock.
- Intrinsic causes: Conditions that directly damage the kidneys, such as glomerulonephritis, pyelonephritis, and interstitial nephritis.
- Postrenal causes: Conditions that obstruct the flow of urine from the kidneys, such as urinary tract infections, kidney stones, and prostate enlargement.
Populations at high risk for developing AKI include:
- Patients with underlying kidney disease
- Patients who are hospitalized
- Patients who are taking nephrotoxic medications
- Patients who are exposed to contrast dyes
The pathophysiology of AKI involves a complex interplay of inflammation and oxidative stress. When the kidneys are injured, they release inflammatory cytokines that can damage the renal tubules and glomeruli. Oxidative stress can also contribute to kidney injury by damaging cellular components.
Clinical Manifestations
The signs and symptoms of AKI can vary depending on the severity of the injury. Common manifestations include:
- Oliguria: Decreased urine output
- Anuria: Complete absence of urine output
- Edema: Swelling in the hands, feet, and ankles
- Nausea and vomiting
- Fatigue
- Confusion
- Seizures
It is important to differentiate between prerenal, intrinsic, and postrenal causes of AKI based on the patient’s history and physical examination. Prerenal AKI is typically caused by hypovolemia or hypotension and can be reversed with fluid resuscitation. Intrinsic AKI is caused by direct damage to the kidneys and may require more intensive treatment, such as dialysis.
Postrenal AKI is caused by obstruction of the urinary tract and can be treated by removing the obstruction.
Diagnostic Evaluation: Nclex Questions Acute Kidney Injury
The diagnosis of AKI is based on a combination of laboratory tests, imaging studies, and a comprehensive patient history and physical examination.
Laboratory tests that are used to diagnose AKI include:
- Serum creatinine: A waste product that is filtered by the kidneys. Elevated serum creatinine levels indicate impaired kidney function.
- Urine output: Decreased urine output is a sign of AKI.
- Blood urea nitrogen (BUN): Another waste product that is filtered by the kidneys. Elevated BUN levels indicate impaired kidney function.
- Electrolytes: Electrolyte imbalances can occur in AKI, such as hyperkalemia and acidosis.
Imaging studies that are used to evaluate AKI include:
- Ultrasound: An ultrasound can be used to visualize the kidneys and urinary tract and to identify any abnormalities.
- CT scan: A CT scan can provide more detailed images of the kidneys and urinary tract than an ultrasound.
Q&A
What are the common causes of AKI?
Common causes include sepsis, hypovolemia, nephrotoxins, and glomerulonephritis.
How is AKI diagnosed?
Diagnosis involves assessing serum creatinine, urine output, and performing imaging studies like ultrasound or CT scans.
What are the goals of AKI treatment?
Treatment aims to restore fluid balance, correct electrolyte imbalances, and manage complications.
What is the role of nurses in caring for patients with AKI?
Nurses monitor fluid balance, electrolytes, and vital signs, prevent and manage complications, and provide education and support.